
Practical strategies and resources for strengthening spinal cord injury care across systems, from community to national level.
Conceptual Framework
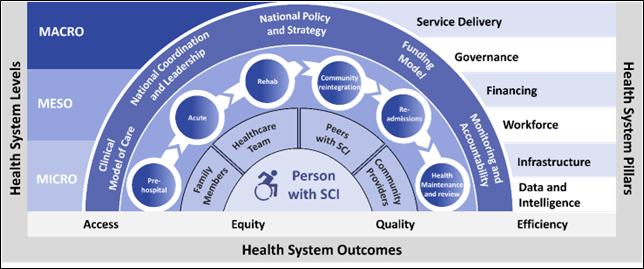
Health Systems Strengthening (HSS) involves improving the performance and impact of a health system through an integrated, multisectoral approach that is flexible, collaborative, practical, and focused on action. Systems Thinking, on the other hand, helps to make sense of complex challenges by recognising how different parts of a system are interconnected. To strengthen the performance and resilience of healthcare systems for improving access, equity, quality, efficiency, and value in SCI services, there must be strong coordination and collaboration among stakeholders at all levels. This requires addressing multiple health system components across the entire continuum of care but adapted to the specific needs, contextual realities, and organisational capacities of countries.
The ISCoS Standards Toolkit offers both an organisational and clinical framework, along with practical guidance for implementation. It supports a comprehensive process of assessment, planning, operationalising and monitoring of SCI Services, whether at a national, subnational, facility or individual patient level. The Toolkit is designed to be flexible and can be used in a range of contexts requiring rapid response or long-term strategic planning. To ensure its effective use, it is essential to consider the broader healthcare system structure that shapes how services are planned, delivered, and managed within a given country or region.
Health System pillars
The six key health system pillars incorporated into the design of the Toolkit are the following:
- Service Delivery: Healthcare services should be accessible to the population and are delivered in an effective and efficient, timely and transparent manner.
- Governance: The provision of clear direction, accountability and oversight within the health system through policies, regulations, legal frameworks, and the appropriate allocation of resources is vital.
- Corporate governance involves setting the overall strategy and policies, delegating responsibilities, overseeing management, and establishing effective risk management and accountability systems across the organisation.
- Clinical governance is an integral part of corporate governance in health service organisations. It ensures that everyone—from frontline clinicians and managers to governing bodies—are accountable to patients and the broader community for delivering health services that are safe, effective, high-quality and continuously improving.
- Financing: The specification of how resources are generated, pooled, allocated and used to fund healthcare services, covering all sources such as public funding, health insurance, and out-of-pocket payments.
- Workforce: The availability, retention and equitable distribution of a skilled, motivated and adequately supported healthcare workforce is crucial.
- Infrastructure: The availability of safe and adequate physical facilities, equipment, assistive technologies, medical supplies, consumables is necessary to support effective healthcare delivery.
- Data and intelligence: A structured and systematic approach to data collection, analysis and use is essential for monitoring outcomes, evaluating health system performance, guiding improvements, informing policy decisions, and and ensuring transparency and accountability.
Health System Structure
For the purposes of these standards for the organisation and delivery of SCI Services, the healthcare system is viewed across three interconnected levels – macro, meso and micro. Care is provided along a continuum, starting from pre-hospital management through emergency and acute care, inpatient rehabilitation, community reintegration, ongoing health maintenance and potential readmissions. Throughout this continuum, a variety of service providers may be involved, operating at different levels of care (such as primary, secondary, or tertiary) and using different modes of delivery, including inpatient, outpatient, outreach, or telemedicine services.
- Macro-level: This level represents broader external factors that influence healthcare systems and impact on healthcare access, delivery and affordability, such as National/sub-national health policies, insurance systems, funding structures and incentives, laws, regulatory mechanisms, geographical factors, including urban-rural distribution, population demographics and socio-economic factors.
- Meso Level: This level focuses on the intermediary structures and organisations within a healthcare system, including clear hospital policies, roles and functions, different services/programmes, networking and relationships between different healthcare and community providers along pathways of care. It includes factors like leadership, cultures, resource allocation, financial and clinical performance, quality improvement, and education and training within these organisations.
The macro and meso levels of a health system interact dynamically, with macro-level policies and structures influencing meso-level practices and decision-making, and vice versa. Macro-level factors, such as national health policies and funding frameworks (e.g., for healthcare coverage or reimbursement rates) establish the basis for meso-level actions, such as hospital governance and resource allocation within organisations for delivering services. Regulations and oversight bodies at the macro level (e.g., government, industry or professional associations) often set standards for quality of care, staffing levels, and other aspects of service delivery, which significantly impact meso-level practices (e.g., within organisations and teams). Meso-level organisations can provide data on service delivery, patient-reported outcomes, and resource utilisation that informs macro-level decision-making and policy development. Meso-level organisations are responsible for implementing and adapting macro-level policies to their local contexts, influencing how those policies are perceived and implemented into practice at the ground level. Meso-level actors, like hospital administrators and community health workers, can advocate for changes in macro-level policies and funding to address specific needs or challenges, such as those experienced by patients with SCI.
- Micro Level: The micro level relates to interactions with person with SCI at an individual level within a specific setting and comprises the interactions between the health professionals, peer mentors, patients, and family. A shared decision-making framework, incorporating best available evidence, professional expertise, patient experiences and preferences, along with use of patient-reported outcome measures supports goal setting, treatment and care planning processes. Micro factors at the level of the team or individual professional include leadership, cultures, relationships, environment, team working, communications, knowledge and training, and continuous quality improvement.
Introduction
Introduction
Spinal cord injury (SCI) due to a traumatic injury or a non-traumatic disease process is a relatively uncommon yet complex disorder, which results in varying degrees of motor impairment, sensory loss and autonomic dysfunction depending on the level and extent of the cord damage. SCI can significantly impact physical functioning, independence, health, psychological wellbeing, and social participation. Access to timely, high-quality, and specialised care is essential to manage impairments, prevent secondary complications and optimise functional recovery and quality of life for the person with SCI.
While the incidence, causes, socio-demographic attributes of SCI vary globally, there is consistent evidence supporting the need for comprehensive, lifelong care delivered by specialised SCI services. These services should address the physical, psychological, social and vocational needs of each individual, aiming to maximise neurological recovery, promote functional independence and support community integration. A coordinated and person-centred approach at every stage across the continuum of care is critical to achieving optimal health, functioning, and quality of life outcomes for every person living with SCI.
The delivery of coordinated SCI care across a continuum is very challenging, particularly in low- and middle-income countries, in which care is often provided in diverse clinical settings where awareness and understanding of SCI may be limited, resources and equipment are lacking, and care pathways are fragmented and poorly coordinated. Therefore, patient management following SCI tends to focus primarily on survival, some basic functional restoration and addressing extensive secondary complications, rather than on proactive prevention of secondary injury and complications, sustainability of long-term health outcomes, quality of life and successful reintegration into society.
Purpose
Purpose – ISCoS Standards Toolkit
The ISCoS SCI Standards Toolkit builds on existing global frameworks and efforts to strengthen health systems, rehabilitation and other services in relation to SCI, by promoting consistent, high-quality, person-centred care. It provides fit-for-purpose practical guidance, along with standards and resources, for developing and strengthening SCI services and systems at a national and subnational level from policy and planning, through operational and services delivery, to monitoring and evaluation across the continuum of care
Target Audience
Target Audience
The primary audience for the Toolkit includes leaders, teams and individuals from government agencies, health authorities, non-government, public and private organisations, service providers, academic institutions or others, involved in policy development, planning, provision or evaluation of SCI services or programmes at a local district, regional or national level. It is also intended for people living with SCI receiving care and family members, relatives or carers who support them. In addition, the Toolkit aims to raise awareness of SCI and support advocacy efforts to improve the availability, quality and accountability of the SCI services provided, in line with best practice principles.
- Government and Service Leaders: The ISCoS Standards Toolkit offers Governments, particularly Ministries of Health (MoH), and Service Leaders with a structured guidance and tools to establish a develop national or local SCI care models aligned with healthcare and rehabilitation policies with healthcare and rehabilitation policies and strategies. It also supports data collection on injury causes, rehabilitation outcomes and long-term health and wellbeing, as well as inclusion for people with SCI in the community. This information can help to inform service planning, funding for value-based care, and the development of injury prevention strategies.
- Healthcare Professionals: The ISCoS Standards Toolkit offers healthcare professionals educational resources to enhance their knowledge, skills and confidence in managing SCI. It includes tools for data collection and outcome measurement to demonstrate the impact of rehabilitation. Implementation of the resource will encourage peer-to-peer collaboration and promote opportunities for multi-centre research.
- SCI not-for-profit and Consumer Organisations: Peer-led organisations or groups often form around SCI Centres or in areas lacking specialised services. They provide vital support, education, advocacy and resources for individuals with SCI and families navigating life after injury and connection through shared experiences, fostering community and empowerment. They offer a variety of services to help participants regain their independence and improve quality of life, whilst promoting awareness and understanding of SCI. The ISCoS Toolkit provides a framework to strengthen both the services these organisations provide and those that they campaign for.
- International Bodies and Agencies: In line with the WHO Rehabilitation 2030 agenda, the WHO is supporting Ministries of Health to develop national strategic plans through its Guide for Action. A key theme emerging from these plans is the urgent need for specialised services for complex conditions, such as SCI and a general increase in inpatient rehabilitation capacity. The ISCoS Toolkit serves as a valuable resource to help Ministries to develop targeted SCI services and support the implementation of National plans and strategies, ultimately improving access to quality care for people with SCI in all levels of the health system.
- NGO/INGOs: The ISCoS Standards Toolkit will assist the Ministry of Health (MoH) in developing a comprehensive National Spinal Cord Injury (SCI) Programme through a structured, evidence-based process. This approach will help identify and define specific areas where support is required—for example, in developing SCI-related infrastructure and services, strengthening the skills and capacity of healthcare professionals, improving systems for data collection and monitoring and promoting SCI-related research. Once these support needs are clearly outlined, they can be systematically incorporated into the planning and implementation of projects by international non-governmental organisations (INGOs) and other development partners, ensuring their contributions align with national priorities and address critical gaps.
- Donor Organisations: The ISCoS Standards Toolkit supports the development of a national or local action plans to strengthen SCI Services based on identified needs, which will require significant funding. Its structured, evidence-based approach can be used to attract donor funding by providing a credible foundation for investment. For donors, this increases the likelihood of achieving lasting system improvements, expanding access to quality care for people with SCI, and potentially creating a model that is transferable to other health conditions.
- People living with SCI and their families: All stakeholders listed above have the common objective of achieving better quality and greater access to comprehensive health and rehabilitation services for people with SCI. The Toolkit promotes understanding of SCI at all levels, supports co-design, planning and delivery of person-centred and needs-based care and enables persons with SCI to use the Toolkit as a resource to advocate for their own rehabilitation journey.
